Key Takeaways
-
Skin pigmentation is controlled by melanin production in melanocytes, with eumelanin producing darker tones and pheomelanin producing lighter tones.
-
Over 125 genes influence skin pigmentation, while environmental factors like UV exposure and hormonal changes can alter melanin production.
-
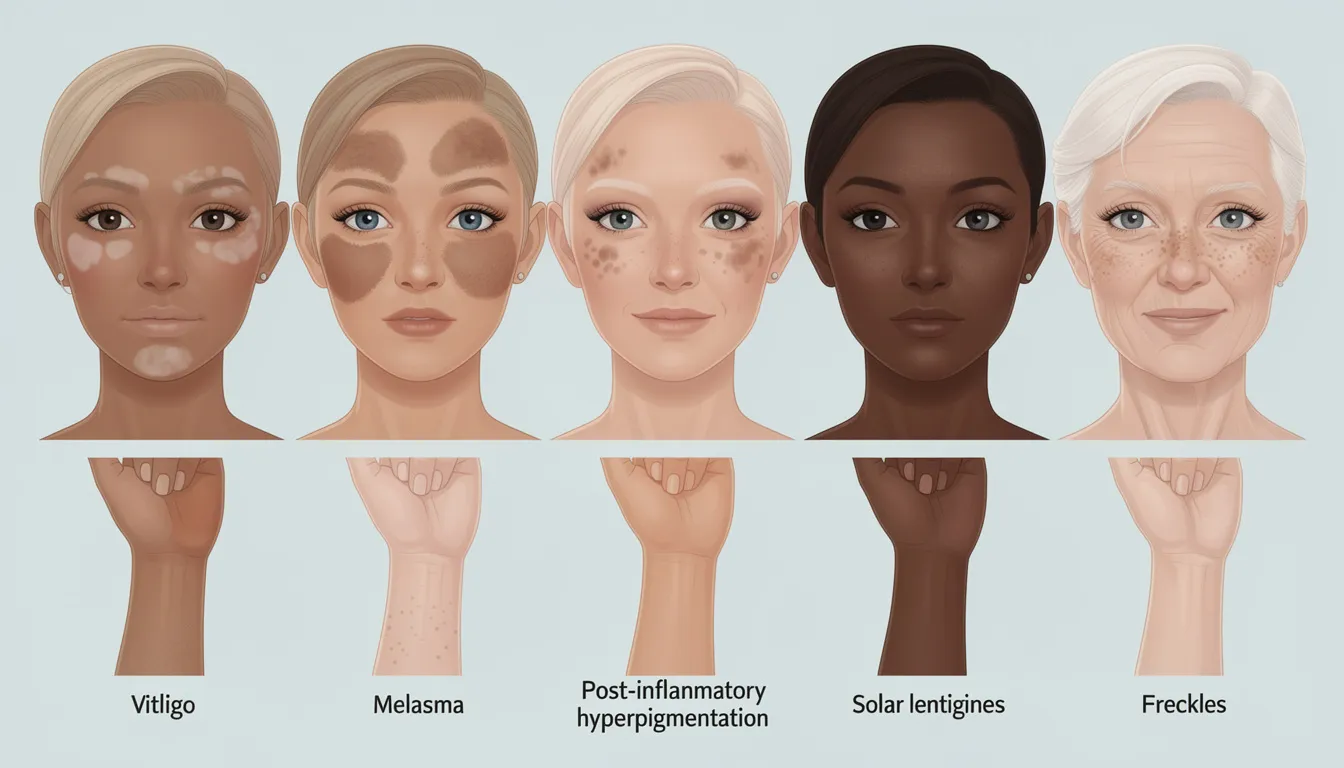
Common pigmentation disorders include melasma, vitiligo, post-inflammatory hyperpigmentation, and solar lentigines, affecting millions worldwide.e
-
Treatment options range from topical hydroquinone and tretinoin to laser therapy and chemical peels, with effectiveness varying by skin type. Pee.
-
Prevention through sun protection and early intervention provides the best outcomes for maintaining healthy skin pigmentation.
Understanding skin pigmentation goes far beyond simple aesthetics—it’s a complex biological process that affects millions of people worldwide. When you’re dealing with dark spots, uneven skin tone, or more serious pigmentation disorders, having comprehensive knowledge about skin color development and changes can empower you to make informed decisions about treatment and prevention.
What is Skin Pigmentation?
Skin pigmentation refers to the coloring of your skin, which is primarily determined by the amount of melanin pigment produced by specialized cells called melanocytes located in the epidermis. These remarkable skin cells act as microscopic factories that produce melanin, creating the pigments that give your skin its unique color and protect it from harmful UV rays.
The human body produces two main types of melanin that determine your natural skin tone. Eumelanin creates brown to black pigmentation and provides excellent photoprotection against sun damage. This type of melanin is more abundant in people with darker skin tones and offers superior defense against skin cancer and other UV-related damage. Pheomelanin, on the other hand, produces red to yellow coloration and is more prevalent in individuals with lighter skin and red hair, though it provides less protection from sun exposure.
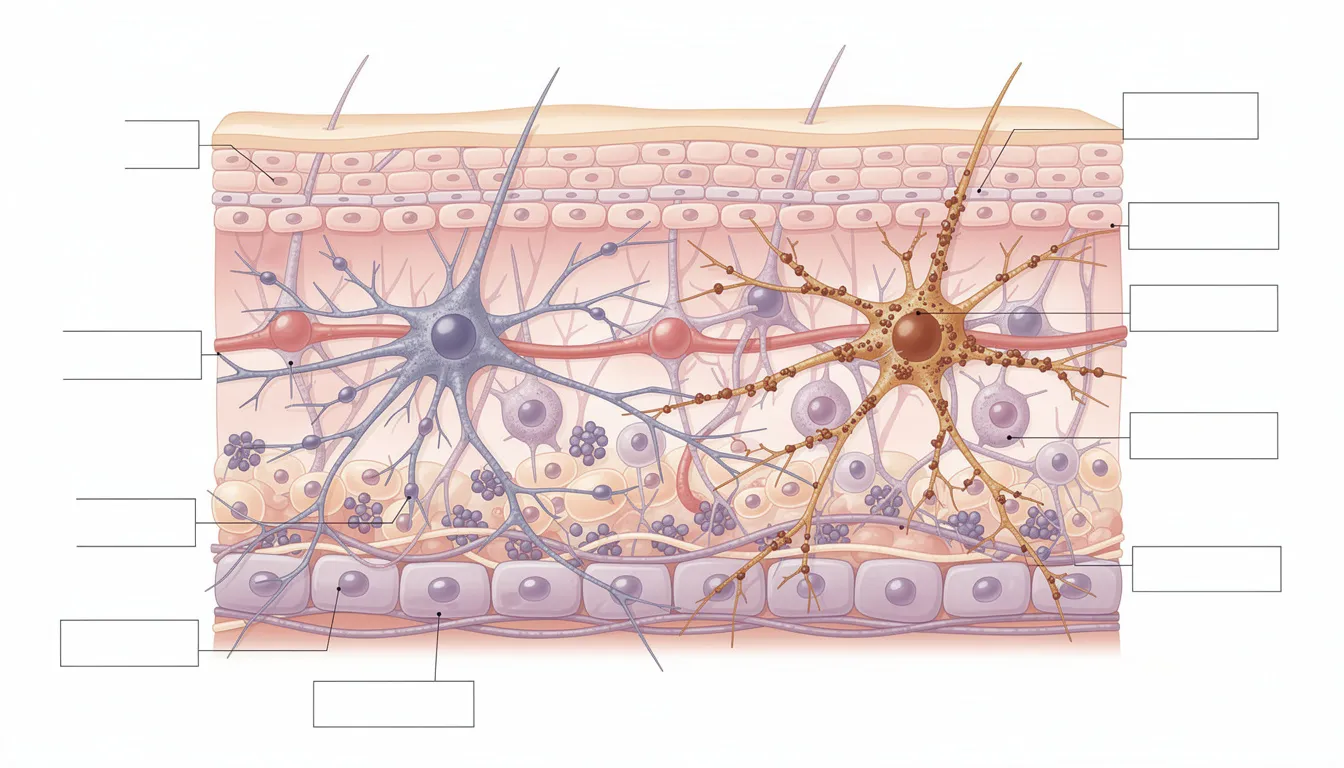
Melanocytes work through an intricate network in which each cell connects with approximately 30-40 neighboring keratinocytes via dendrite-like extensions. This creates what scientists call" the melanocyte unit,” where melanin-containing organelles called melanosomes are transferred from melanocytes to surrounding skin cells, forming protective caps over cell nuclei to shield DNA from radiation damage.
The amount of melanin your body produces naturally determines your baseline skin color, but various factors can change it over time. Normal variations in skin pigmentation across different ethnicities reflect thousands of years of evolutionary adaptation to different UV exposure levels, with people in high-sun environments having more melanin as a protective adaptation, while lighter skin facilitates vitamin D synthesis in regions with limited sunlight.
The Science Behind Melanin Production
The process of melanin production, known as melanogenesis, is one of the most sophisticated biochemical pathways in the human body. At its core, this process begins when specialized cells called melanocytes respond to various signals by activating the enzyme tyrosinase, which is the rate-limiting step in converting the amino acid tyrosine into melanin.
The enzyme tyrosinase plays a crucial role as the primary catalyst in this conversion process. It first hydroxylates tyrosine to form L-DOPA, then oxidizes L-DOPA to form DOPAquinone. From this point, the pathway diverges based on the cellular environment. In the presence of cysteine and glutathione, it leads to pheomelanin formation, whereas their absence directs it toward eumelanin synthesis via additional enzymatic steps involving TYRP1 and TYRP2.
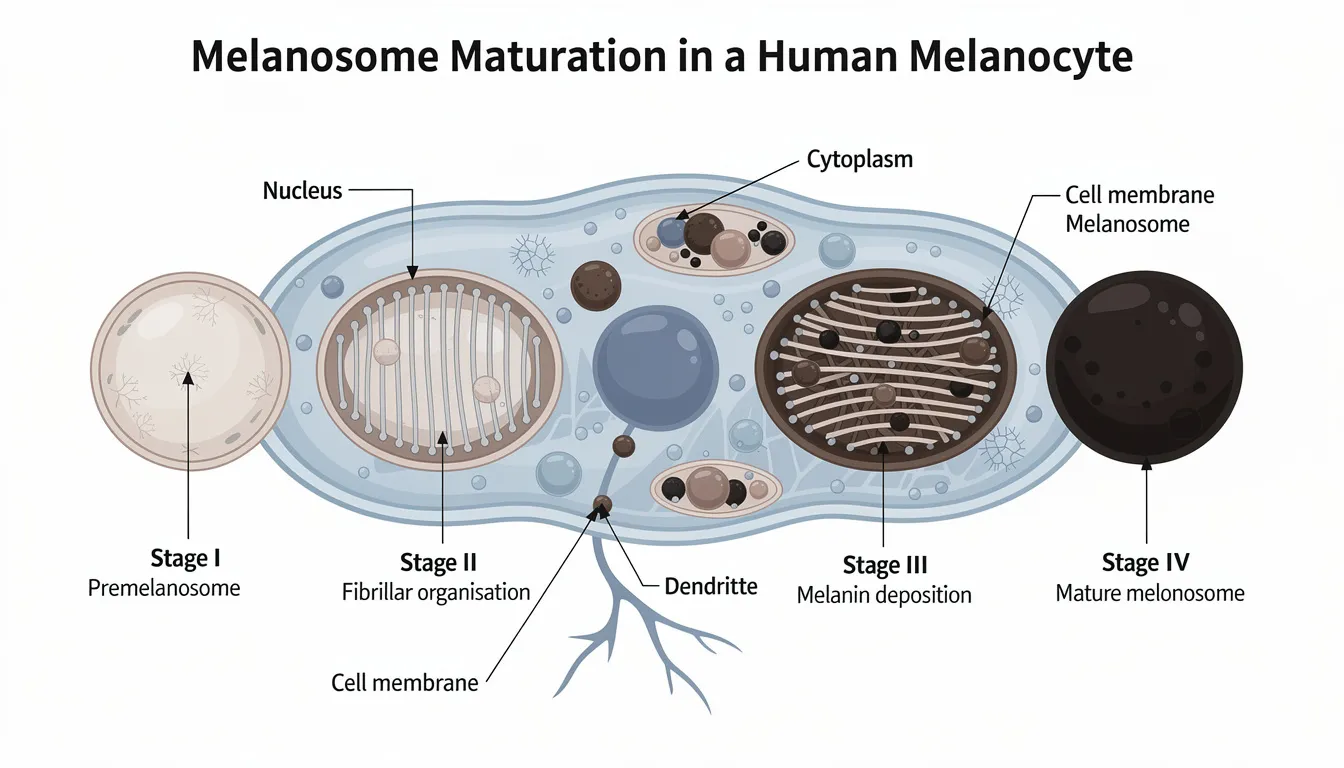
Melanosomes, the organelles where melanin synthesis occurs, mature through four distinct stages. They begin as simple vesicles, develop fibrillar matrices, accumulate melanin deposits, and finally become fully melanized organelles ready for transfer. The transfer process from melanocytes to keratinocytes occurs through several mechanisms, including phagocytosis of dendrite tips and specialized membrane tunneling, ensuring even distribution of protective pigment throughout the epidermis.
The MC1R gene acts as a master switch in regulating this entire process. When activated by hormones like α-melanocyte-stimulating hormone (α-MSH), it triggers a cascade of cellular events that increase both the quantity and quality of melanin production. Variations in MC1R function explain much of the natural diversity in human skin color, with specific polymorphisms strongly associated with red hair, fair skin, and increased UV sensitivity.
Hormonal influences add another layer of complexity to melanin production. Adrenocorticotropic hormone (ACTH) and melanocyte-stimulating hormone (MSH) can dramatically increase pigmentation, which explains why conditions such as Addison’s disease often present with generalized skin darkening. These hormonal pathways also account for pregnancy-related pigmentation changes and the effectiveness of certain hormonal contraceptives in triggering melasma.
Primary Causes of Skin Pigmentation Changes
Skin color changes result from a complex interplay of genetic programming, environmental exposures, and medical factors. Chemical exposure can trigger pigmentation changes by increasing melanin synthesis or causing skin injury. Additionally, poor healing after wounds or burns can result in persistent pigmentation changes. Understanding these various causes helps explain why some people develop certain pigmentation disorders while others remain unaffected, and guides appropriate treatment selection.
Genetic Factors
More than 125 genes work together to control melanin production and distribution, making skin pigmentation one of the most polygenic traits in humans. These genes influence everything from the basic structure of melanosomes to the efficiency of melanin transfer between cells, creating the remarkable diversity of human skin tones observed worldwide.
Inherited variations in genes like MC1R, SLC24A5, and OCA2 determine your baseline skin tone and influence how your skin responds to environmental triggers. Family history patterns often predict susceptibility to specific pigmentation disorders, with conditions like melasma showing strong familial clustering, particularly among women of Hispanic and Asian descent.
Ethnic predispositions to specific conditions reflect both genetic ancestry and evolutionary adaptations. For example, people of African descent typically have more efficient melanogenesis and larger, more individually dispersed melanosomes, providing better photoprotection but potentially increasing susceptibility to post-inflammatory hyperpigmentation following skin injuries or inflammation.
Environmental Influences and Sun Exposure
UV radiation is the most significant environmental trigger of pigmentation changes. The body produces melanin as a protective response to sun exposure, with UVB radiation (290-315 nm) being particularly effective at stimulating delayed tanning responses through DNA damage pathways that activate melanocyte function.
Seasonal changes create predictable patterns in melanin production, with most people experiencing lighter skin during winter months and progressive darkening throughout summer. Geographic location plays a crucial role: individuals living closer to the equator tend to maintain higher baseline pigmentation levels due to consistent UV exposure year-round.
Occupational sun exposure presents unique risks for certain professions. Outdoor workers, pilots, and individuals with significant window exposure often develop asymmetric pigmentation patterns, with more pronounced changes on the left side of the face from driving or specific body areas based on work positioning.
Medical and Hormonal Factors
Pregnancy-related pigmentation changes, known as chloasma o" the “mask of preg"ancy,” affect up to 70% of pregnant women due to elevated estrogen and progesterone levels. These hormones enhance melanocyte sensitivity to UV exposure and can trigger melanin production even in previously unaffected individuals. Birth control pills containing similar hormones can produce identical effects.
Medication-induced pigmentation represents a significant category of acquired skin discoloration. Antibiotics like minocycline can cause blue-gray pigmentation in sun-exposed areas, while antimalarials may produce characteristic patterns around the eyes and in the mouth. Other medications, including specific chemotherapy agents and psychotropic drugs, can also alter skin color by directly depositing pigment or by affecting melanin synthesis pathways.
Endocrine disorders frequently manifest through pigmentation changes. Addison’s disease typically causes generalized hyperpigmentation due to elevated ACTH levels. In contrast, thyroid disorders can subtly influence skin color by altering melanocyte function. Additionally, inflammatory skin conditions like atopic dermatitis often lead to post-inflammatory changes that can persist long after the original condition resolves.
Common Pigmentation Disorders
Pigmentation disorders fall into two main categories: hyperpigmentation, where excess melanin creates darker areas, and hypopigmentation, where melanin deficiency results in lighter patches of skin. These pigmentation disorders are a type of skin disease and part of a broader group that affects the skin's appearance and health. Each category encompasses distinct conditions with specific characteristics, triggers, and treatment approaches. Additionally, skin rashes and other inflammatory skin conditions can lead to pigmentation changes, further linking pigmentation disorders to a wide range of skin conditions.
Hyperpigmentation Conditions
Melasma affects approximately 6 million American women, presenting as symmetric, dark-brown patches primarily on the face. This condition shows strong associations with hormonal changes, particularly pregnancy and oral contraceptive use, earning it the nickname “pregnancy mask.” The condition predominantly affects women of childbearing age with darker skin tones, and UV exposure significantly worsens existing lesions. Melasma treatment options include topical agents such as tranexamic acid and systemic medications like isotretinoin, which have shown efficacy in reducing pigmentation changes. Post-inflammatory hyperpigmentation commonly develops following acne lesions, eczema flares, or other inflammatory skin conditions. This condition disproportionately affects individuals with darker skin tones due to more reactive melanogenesis and tends to be more severe and longer-lasting in these populations. These conditions often present as dark skin patches. The darkened areas can persist for months to years without proper treatment and sun protection.
Solar lentigines, commonly called age spots or liver spots, affect approximately 90% of people over 60 years old in sun-exposed areas. These flat, dark brown spots result from years of cumulative UV exposure and represent areas of increased melanocyte activity and proliferation. Sun spots are a common form of hyperpigmentation caused by sun exposure. Unlike freckles, which fade in winter, solar lentigines persist year-round and tend to increase in number and size over time.
Café-au-lait macules appear as light brown, flat spots and are present in 10-20% of the normal population. While usually benign, multiple large café-au-lait macules may indicate underlying genetic conditions, such as neurofibromatosis. These lesions typically remain stable throughout life unless associated with systemic conditions.
Drug-induced hyperpigmentation can result from various medications, including antimalarials, which often cause blue-black discoloration in sun-exposed areas, and minocycline, which may produce distinctive blue-gray pigmentation. Chemotherapy agents can also cause diffuse hyperpigmentation or characteristic nail and mucosal changes.
When over-the-counter options are insufficient, prescription creams are often used to help restore skin tone and reduce persistent dark patches.
Hypopigmentation Conditions
Vitiligo affects 0.5-2% of the global population and is an autoimmune condition in which the immune system attacks and destroys melanocytes. This results in well-demarcated white patches that can appear anywhere on the body but commonly affect the face, hands, and areas around body openings. The condition often progresses unpredictably and can have a significant psychological impact, particularly in individuals with darker skin, where the contrast is more pronounced.
Albinism represents a group of genetic conditions with an estimated prevalence of 1 in 17,000 worldwide, though rates can be much higher in specific populations due to founder effects. These conditions involve mutations in genes essential for melanin synthesis, resulting in absent or severely reduced pigmentation in skin, hair, and eyes. People with albinism face extremely high risks of skin cancer and require lifelong photoprotection.
Pityriasis alba commonly affects children, particularly those with atopic dermatitis, appearing as scaly, hypopigmented patches primarily on the face and arms. These lesions typically resolve spontaneously over months to years but may require moisturization and mild topical therapies to speed recovery.
Tinea versicolor, caused by an overgrowth of naturally occurring skin yeast, creates distinctive hypopigmented or hyperpigmented patches with fine scaling. This fungal infection commonly affects adolescents and young adults, particularly in warm, humid climates, and often recurs seasonally despite successful treatment.
Chemical-induced hypopigmentation can result from exposure to specific bleaching agents, industrial chemicals, or even some topical medications. Permanent melanocyte damage may occur with severe exposures, making prevention through proper handling and protective equipment essential for at-risk individuals.
Impact of Skin Discoloration
We understand that skin discoloration touches so much more than what you see in the mirror—it can quietly chip away at your confidence and change how you move through your day. When uneven skin tone, dark spots, or patches appear, we know how deeply personal and isolating that can feel. Those moments of catching your reflection and feeling uncertain, or choosing different clothes to feel more comfortable—we see you, and we want you to know that these feelings aren't entirely invalid. Your skin tells a story, and every part of that story matters. We've learned over the years that your skin is often trying to tell you something important. Those persistent dark areas or changes in skin's natural tone aren't just surface concerns; they're skin's way of asking for attention and care. Sometimes these changes happen after your skin has been through something difficult, like healing from breakouts or responding to irritation, and that healing process can take time, patience, and the right kind of gentle support. We believe in listening to what your skin truly needs rather than rushing to cover up; it's trying to communicate.
This is why we approach skin care with such intention and respect for skin's natural wisdom. A person's skin has its own story and needs a thoughtful solution; there's no one-size-fits-all, and we wouldn't want it to be. Whether it's through gentle, nourishing products made with ingredients your skin recognizes, or connecting you with the right kind of professional guidance, we believe in taking the time to understand what will truly serve you. Your skin deserves to be as individual as you are; we're honored to be part of that journey toward feeling comfortable and confident in your own skin.
Understanding Dark Skin
We believe that darker skin tones are beautifully designed with increased melanin, nature's own thoughtful way of offering protection against the sun's harsh UV rays. This higher concentration of melanin acts as a gentle shield, protecting your skin from sun damage and naturally lowering the risk of certain skin cancers. Yet this same melanin that provides such excellent protection can sometimes make those with deeper skin tones more sensitive to pigmentation concerns, such as hyperpigmentation and stubborn dark spots that linger longer than we'd like.
When it comes to addressing hyperpigmentation in darker skin, we sincerely believe in taking a careful, personalized approach — one that truly honors what your skin needs. While treatments like topical corticosteroids, chemical peels, and laser therapy are often recommended for skin discoloration, we know these must be chosen and applied with genuine intention and care. Darker skin responds best to thoughtful treatment, but it's more prone to developing further discoloration when aggressive approaches are used. That's why we always recommend starting with gentler options and moving at a slower, more mindful pace while closely watching how your skin responds.
Natural remedies like aloe vera and kojic acid have become beloved staples for their ability to reduce hyperpigmentation with genuine gentleness, promoting that even skin tone we're all seeking. Vera's deeply soothing, anti-inflammatory properties calm and comfort irritated skin, while kojic acid thoughtfully lightens dark spots by gently inhibiting melanin production. When we take time to truly understand the unique needs of darker skin tones and choose treatments that feel honest and effective, we can beautifully manage pigmentation concerns and maintain healthy, radiant skin that glows with natural vitality, even with regular sun exposure.
Treatment Options for Pigmentation Disorders
Effective treatment of skin pigmentation disorders requires a comprehensive approach tailored to the specific condition, skin type, and severity. For more severe or persistent pigmentation disorders, prescription creams are available and may be recommended by dermatologists. Treatment success depends heavily on early intervention, consistent application, and appropriate selection of modalities based on individual patient factors.
Advanced procedures for hyperpigmentation include laser treatment, a dermatologist-supervised procedure effective for cosmetic improvement of conditions such as melasma and solar lentigines. Light therapy, including intense pulsed light (IPL), is also an option for treating pigmentary disorders and superficial skin lesions. However, it is essential to note that light treatment, such as laser or IPL, can sometimes induce or worsen pigmentation issues, particularly in individuals with darker skin types.
The evidence supporting the efficacy and safety of specific therapies, such as hydroquinone for hyperpigmentation and ruxolitinib cream for vitiligo, is based on randomized controlled trials that demonstrate their clinical effectiveness and tolerability.
Topical Medical Treatments
Hydroquinone remains the gold standard for treating hyperpigmentation, available in concentrations ranging from 2-4%. This agent inhibits tyrosinase activity and can cause oxidative damage to melanocytes at higher concentrations. While highly effective, hydroquinone requires careful monitoring due to potential side effects, including irritant contact dermatitis and paradoxical darkening in some patients, particularly those with darker skin.
Topical tretinoin, available in concentrations from 0.025-0.1%, enhances cellular turnover and improves penetration of other agents. This retinoid normalizes keratinocyte differentiation and accelerates the removal of pigmented cells from the outer layer of skin. Tretinoin synergizes with hydroquinone and is often prescribed in combination formulations to enhance efficacy.
Kojic acid and azelaic acid are effective alternatives to hydroquinone for patients who cannot tolerate it. Kojic acid chelates copper ions essential for tyrosinase function, while azelaic acid provides additional anti-inflammatory benefits that help prevent post-inflammatory hyperpigmentation. These agents typically cause less irritation than hydroquinone but may require more extended treatment periods to achieve comparable results.
Combination therapies like Tri-luma, which contains hydroquinone, tretinoin, and a mild corticosteroid, can provide enhanced efficacy, while the steroid component helps minimize irritation. Kligman’s formula represents another popular combination approach, though it requires careful compounding and monitoring due to potential side effects from prolonged steroid use.
Topical corticosteroids play a specific role in treating inflammatory pigmentation, particularly in acute post-inflammatory hyperpigmentation. However, long-term use must be avoided due to risks of skin atrophy, striae formation, and paradoxical hyperpigmentation, especially in skin of color.
Oral Medications
Tranexamic acid, typically prescribed at 250-500mg daily, has emerged as an effective treatment for melasma, particularly in cases resistant to topical therapies. This medication works by blocking plasmin-induced melanocyte activation and has shown success rates of 60-80% in clinical trials. Treatment duration usually ranges from 3 to 6 months, with maintenance therapy sometimes required.
Oral antifungals are the primary treatment for tinea versicolor, with medications such as fluconazole or itraconazole effectively eliminating the causative yeast. These treatments typically require short courses of 1-2 weeks, though recurrence is common and may require prophylactic dosing in susceptible individuals.
Supplements including vitamin C, vitamin E, and niacinamide may provide modest benefits in treating hyperpigmentation through their antioxidant properties. While evidence for their effectiveness remains limited, these supplements have excellent safety profiles and may complement other treatment modalities.
Systemic treatments for underlying inflammatory conditions, such as atopic dermatitis or autoimmune disorders, can help prevent pigmentation changes by controlling the underlying inflammatory process. This approach proves particularly valuable in preventing recurrent post-inflammatory hyperpigmentation.
Advanced Procedures
Chemical peels with glycolic acid at concentrations of 20-70% provide controlled removal of pigmented surface layers. These procedures accelerate cellular turnover and can be particularly effective for superficial pigmentation. However, deeper peels carry a higher risk of scarring and paradoxical hyperpigmentation, especially in darker skin types.
Laser therapy offers targeted treatment for specific pigmentation types. Q-switched lasers deliver short, intense pulses of light that selectively destroy melanin-containing cells while sparing surrounding tissue. These treatments typically require multiple sessions spaced 4-6 weeks apart and can achieve excellent results for solar lentigines and some types of melasma.
Cryotherapy using liquid nitrogen provides an effective treatment for solar lentigines and other benign pigmented lesions. This procedure causes controlled tissue destruction through freeze-thaw cycles, typically resulting in lesion resolution within 2-4 weeks. However, hypopigmentation can occur, particularly in darker skin types.
Microneedling combined with vitamin C or other lightening agents can enhance the penetration and effectiveness of topical treatments. This procedure creates controlled micro-injuries that stimulate cellular renewal while allowing deeper penetration of active ingredients.
Intense pulsed light (IPL) treatment uses broad-spectrum light to target melanin and can effectively treat diffuse pigmentation issues. Multiple sessions are typically required, and careful parameter selection is essential to avoid complications in darker skin tones.
Natural and Alternative Remedies
Plant-based ingredients offer gentler alternatives for those seeking to address pigmentation concerns without harsh chemicals. Many of these natural compounds work through tyrosinase inhibition, antioxidant activity, or by promoting healthy cellular turnover. Certain natural oils, such as jojoba and argan oil, are especially beneficial for dry skin, as they help improve skin hydration, flexibility, and barrier function while supporting overall skin health.

Vitamin C serums containing 10-20% L-ascorbic acid provide both brightening and antioxidant benefits. This essential nutrient reduces melanin production by inhibiting tyrosinase activity and helps fade dark spots through its antioxidant properties—stable vitamin C derivatives, such as magnesium ascorbyl phosphate, offer similar benefits with less potential for irritation.
Licorice root extract contains glabridin, a powerful compound that inhibits tyrosinase activity without causing cytotoxicity to melanocytes. This natural lightening agent works particularly well for inflammatory hyperpigmentation and has anti-inflammatory properties that help prevent further pigmentation while treating existing spots.
Green tea polyphenols, particularly epigallocatechin gallate (EGCG), provide potent antioxidant protection that helps prevent UV-induced pigmentation. These compounds also have direct tyrosinase inhibitory activity and can be applied topically or consumed as supplements for systemic benefits.
Arbutin, derived from bearberry plants, acts as a natural alternative to hydroquinone by slowly releasing hydroquinone upon absorption into skin cells. This gradual release provides the benefits of hydroquinone with significantly less irritation, making it suitable for sensitive skin types and long-term use.
Turmeric contains curcumin, which provides both anti-inflammatory and mild skin brightening effects. While not as potent as other natural lightening agents, turmeric offers additional benefits for overall skin health and can be particularly useful for preventing post-inflammatory hyperpigmentation. Kojic acid, derived from rice fermentation, provides another natural option with proven tyrosinase-inhibitory activity.
Aloe vera offers soothing and healing properties that can help prevent post-inflammatory hyperpigmentation while providing mild brightening effects. The anti-inflammatory properties of aloe vera help calm irritated skin and support the healing process after procedures or inflammatory skin conditions.
Prevention and Daily Management
Effective prevention represents the most crucial strategy for maintaining healthy skin pigmentation and preventing disorders before they develop. A comprehensive approach combining sun protection, appropriate skincare, and lifestyle modifications provides the best long-term outcomes.
Sun protection strategies form the cornerstone of pigmentation prevention. Daily application of broad-spectrum SPF 30+ sunscreen provides essential protection against both UVA and UVB radiation. Reapplication every 2 hours, or immediately after swimming or excessive sweating, ensures maintained protection throughout the day. Many patients underestimate the amount of sunscreen needed—approximately 1/4 teaspoon for the face and neck alone. In addition to sunscreen, avoiding sun exposure whenever possible is a key preventive measure to reduce hyperpigmentation and prevent existing spots from darkening.
Physical barriers complement chemical sun protection effectively. Wide-brimmed hats with at least 4-inch brims provide significant protection for the face, neck, and ears—areas commonly affected by sun damage. UV-protective clothing with UPF ratings offers reliable protection for the body, particularly during outdoor activities or in high-UV environments.

Skincare routine adaptations for pigmentation-prone skin should emphasize gentle, non-irritating products that support healthy cellular turnover without causing inflammation. Regular use of gentle exfoliating agents, such as salicylic acid, can help prevent clogged pores that may lead to inflammatory acne lesions and subsequent hyperpigmentation. Moisturizers with niacinamide provide additional benefits by reducing inflammation and supporting barrier function.
Lifestyle modifications play a crucial role in preventing hormonal triggers for conditions like melasma. Women with a history of pregnancy-related pigmentation should discuss contraceptive options with their healthcare providers, as some birth control pills may exacerbate existing pigmentation. Stress management techniques may also help, as stress hormones can influence melanocyte activity.
Regular dermatological monitoring enables early detection and intervention for pigmentation changes. Annual skin examinations allow for the identification of new lesions and the monitoring of existing pigmented spots for changes that might indicate malignancy. Patients with risk factors for pigmentation disorders should consider more frequent monitoring.
Early intervention strategies provide the best opportunities for successful treatment outcomes. Addressing inflammatory skin conditions promptly helps prevent post-inflammatory hyperpigmentation, while starting treatment for conditions like melasma during the early stages typically yields better results than treating established, long-standing pigmentation.
Emerging Trends in Skin Pigmentation Treatment
At our practice, we believe treating skin pigmentation should feel thoughtful, deeply personal, and intentional. Laser therapy has become one of our most cherished approaches because it allows us to work with precision and care, targeting those stubborn areas you've been concerned about while remaining genuinely gentle to the surrounding skin. We love how this treatment honors what your skin truly needs — focused attention on areas that matter most to you, with results that feel both noticeable and natural. There's something beautiful about offering you solutions that work with your skin rather than against it.
When we talk with clients about topical therapies like salicylic acid and tretinoin, we're always moved by how these simple, time-tested ingredients can transform your daily routine. aren'taren't trendy additions or flashy extthey'rehey're honest, effective choices that help your skin renew itself by gently encouraging cell turnover and working beautifully alongside other treatmWe've We've seen how combining these thoughtful topical options with laser therapy creates results that feel both comprehensive and personal, improving not just individual spots but your overall skin tone in ways that make you feel confident and cared for.
One of our favorite parts of this work is witnessing how natural remedies like aloe vera and green tea are earning their rightful place in serious skincare conversations. These ingredients offer anti-inflammatory properties we genuinely respect — they soothe and support skin's healing process with the kind of gentle effectiveness that never goes out of style. As we continue learning about the beautiful complexity of melanin production and skin pigment patterns, we're excited about creating treatment plans that honor both advanced medical options and nature's own wisdom. When you choose to work with your practitioners, you're selecting practitioners who believe in quality over quick fixes, intention over industry trends, and comprehensive care that sees your whole skin story.
FAQ
How long does it take to see results from pigmentation treatments? Most topical treatments require 3-6 months of consistent use to show visible improvement, while laser treatments may show results after 2-4 sessions spaced 4-6 weeks apart. However, results vary significantly based on the condition type, skin type, and treatment compliance. Post-inflammatory hyperpigmentation may fade more quickly than melasma, which often requires more extended treatment periods and maintenance therapy.
Can skin pigmentation disorders be completely cured? While some conditions, such as post-inflammatory hyperpigmentation, can resolve completely with appropriate treatment, others ass, such as melasma and vitiligo, require ongoing management. Success rates vary from 60% to 90% improvement depending on the condition and treatment approach. A complete cure is possible for infectious causes such as tinea versicolor, but genetic conditions typically require lifelong management strategies.
Are there any risks associated with pigmentation treatments? Yes, potential risks include skin irritation, paradoxical hyperpigmentation (especially in darker skin tones), scarring from aggressive treatments, and allergic reactions to topical ingredients such as hydroquinone. Laser therapy carries risks of permanent pigmentation changes if not performed correctly. It’s essential to work with qualified dermatologists who understand how different treatments affect various skin types.
Which skin types are most prone to pigmentation problems? Fitzpatrick skin types III-VI (olive to dark skin) are more susceptible to post-inflammatory hyperpigmentation and melasma due to more reactive melanogenesis. However, types I-II (fair skin) are more prone to sun damage, solar lentigines, and age spots. Each skin type faces different pigmentation challenges that require tailored prevention and treatment approaches.
Can diet affect skin pigmentation? While it doesn’t directly change melanin production, antioxidant-rich foods containing vitamin C, vitamin E, and beta-carotene may help protect against UV-induced pigmentation. Some foods high in psoralens (like celery, limes, and figs) can increase photosensitivity and potentially worsen existing pigmentation when combined with sun exposure. A balanced diet supports overall skin health, helping achieve more even pigmentation over time.
Conclusion
We know that skin pigmentation concerns, whether you're dealing with hyperpigmentation or hypopigmentation, can really affect how you feel about yourself, and we truly understand how important confidence is. We believe that getting to the heart of what's causing your skin discoloration is the first step toward finding the right path forward. Whether you're drawn to gentle topical treatments, considering laser therapy, or exploring natural remedies that feel more aligned with your values, there are thoughtful ways to address hyperpigmentation, help those stubborn dark spots and age spots fade, and work toward that even skin you're hoping for.
We always encourage taking a caring, comprehensive approach to managing skin pigmentation that puts sun protection at the center of everything. Those UV rays can be real troublemakers when it comes to triggering pigmentation issues. We're big believers in avoiding excessive sun exposure and being mindful about protection. Using gentle, non-irritating products that respect skin's natural processes, and following a treatment that's been thoughtfully created just for you, show you how to prevent further damage while supporting skin's long-term health and happiness.
One thing we love is when people stay curious and informed about the latest advances in skin pigmentation treatments. It's empowering, isn't it, knowing you can make the best choices for your unique skin? If you notice changes like new dark spots, age spots, or any unusual patches that concern you, we always encourage you to reach out to a healthcare professional who can provide an accurate diagnosis and create a treatment tailored just for you. With proper care, the proactive steps you're taking, and a little patience, you can reduce your risk of skin discoloration and nurture healthy, radiant skin that lasts for years to come.





